|
* Petrov et al.
|
2018 |
Observational |
7 d actigraphy and diary with self-report measures. |
760 Com |
Hispanic |
46.8 (10.4) |
61.2% |
7 |
Actigraphy (with Diary) |
ISD |
A |
A: Commute time (short, moderate, long) |
Multiple jobs, work hours, depression, anxiety, caffeine, age, sex, income. |
- TSTv: moderate > short commuters, nonsig b/w long and short comuters.
|
|
* Chung et al.
|
2018 |
Observational |
7 d actigraphy and diary with self-report and neurocognitive measures. |
66 schizophrenia |
Chinese |
44.08 (12.64) |
54.54% |
7 |
Actigraphy and Diary |
Square of Successive Difference |
C |
C: schizophrenia symptoms, depression, sleepiness, social rhythm, chronotype, DSPD, caffeine and dinner time, cigarette, hypnotics and antipsychotics use, number of times of pencil-off paper during neurocognitive assessment. |
None. |
- Acti: +TIBv & +TSTv ~ later caffeine, DSPD, social rhythm irregularity; +TSTv ~ -hypnotic dose; +SOLv ~ later caffeine,-hypnotic dose; -SOLv ~ combination of first- & second generation antipsychotics; +WASOv ~ -antipsychotic dosage; +SEv ~ secondary education, later dinner, social rhythm irregularity, -hypnotic dose.
- Diary: +BTv ~ social rhythm irregularity, -pencil-off-paper in cognitive tasks; +WTv ~ DSPD, +depression, social rhythm irregularity; +SOLv ~ DSPD, +depression, +eveningness; +WASOv ~ -pencil-off-paper in cognitive task; +SEv ~ DSPD, +eveningness, social rhythm irregularity; +TSTv ~ DSPD, +positive symptoms, social rhythm irregularity; +Qualityv ~ +cigarette, DSPD, +positive symptoms, +sleepiness, +eveningness, social rhythm irregularity.
|
|
* Chan et al.
|
2018 |
Observational |
14 d actigraphy and diary with self-report measures. |
223 adults fibromyalgia & insomnia |
79.6% White, 17.4% Black |
51.87 (11.75) |
93.70% |
14 |
Actigraphy (with Diary) |
ISD |
A, B, C, D. |
A: demographics, caffeine; B: pain; sleep medication; C: depression, anxiety, fatigue; D: unhelpful sleep beliefs. |
None. |
- "DV" refers to sleep discrepancy (actigraphy vs diary) IIV;
- SOL-DV: NS with all correlates;
- WASO-DV ~ +pain, +pain medication, +caffeine;
- TST-DV ~ +depression, +pain & sleep medication, +caffeine;
- DV IIV and unhelpful sleep beliefs NS.
|
|
* Xu et al.
|
2018 |
Observational |
Fitbit Charge HR based actigraphy and up to 3 times of health/blood tests over 12 months. |
471 Com |
NR (US) |
49.7 |
51.3% |
Average 78.2 |
Actigraphy |
ISD |
A, B |
A: sex, age, season, day of the week; B: BMI, blood pressure, blood test. |
Sex, age, geographic location, genetic ancestry; habitual sleep duration. |
- TSTv ~ +BMI (control for TSTm), winter season & weekends. NS difference b/w sex, but female ~ +magnitude of mean TSTv annually;
- TSTv ~ + total white blood cell count, +absolute neutrophil count, but both NS after correcting for multiple comparisons.
- NS b/w long/short-term IIV and blood pressure;
|
|
* Whitesell et al.
|
2018 |
Observational |
Data collected when infants were 1, 3, 6, 9, and 12 months. Actigraphy, questionnaire, interviews, and video recordings. |
167 Com |
Mothers: 84% White, Fathers: 84% White |
Mothers: 29.43 (5.27). Fathers: 32.10 (5.87) |
~50% (parent dyads) |
7 |
Actigraphy with daily phone interviews. |
NR |
A |
A: household chaos & infant care |
Mothers' reports of marital adjustment. |
- Household chaos ~ +IIV of sleep timing and TSTv (mothers & fathers), Fragmentationv(fathers not mothers);
- Infant age ~ decreased TSTv (fathers not mothers);
- See paper for interaction between chaos and infant age on sleep IIV.
|
|
* Molzof et al.
|
2018 |
Observational |
Archival data from epidemiological survey |
723 Com |
69.8% White, 28.9% Black |
53.8 (19.8) |
50.6% |
14 |
Diary |
ISD |
D |
D: good/poor sleeper, sleep complaint |
Age, sex, race |
- Poor sleep ~ +TSTv, +SOLv, +WASOv, +WASOnv, +SEv;
- See paper on details of poor sleep x sleep complaint interaction on sleep IIV.
|
|
* Kuula et al.
|
2018 |
Observational |
Actigraphy and cognitive tests from a cohort study |
322 Com |
NR (FI) |
25.3 (0.65) |
55.7% |
7 |
Actigraphy |
ISD |
C |
C: Executive function |
Age, sex, BMI, education |
- Higher TSTv ~ poorer motoric performance (small) but better complex processing (small)
|
|
* Yetish et al.
|
2018 |
Observational |
Data from randomly sampled Tsimane adults 40+ age |
120 Tsimane adults |
Tsimane |
Male: 42.3 (15.9); Female: 38.3 (15.7) |
55.83% |
7 (3-10) |
Actigraphy with interviews |
ISD |
A |
A: sex |
Day of the week, sex, TSTm, nighttime activities |
- TSTv: male > female;
- Both male and femal: SOTv > WTv.
|
|
* Wallace et al.
|
2018 |
Observational |
Actigraphy and self-report health |
2887 Com (older) |
89.9% White |
76.3 (5.5) |
0% |
Average 5.3 |
Actigraphy |
ISD |
B |
B: Mortality risk |
Sleep and non-sleep risk factors |
- WTv ~ +mortality risk in the univariable models but not in multivariable model.
|
|
* Lunsford-Avery et al.
|
2018 |
Observational |
Data from longitudinal cohort study, sleep measured 10 years prior to health measures. |
1978 Com (older) |
39% White, 28% Black, 23% Hispanic |
68.7(9.2) |
54% |
7 |
Actigraphy with diary |
SRI |
A, B, C |
A: age, sex, race, education, employment, light exposure; B: cardiovascular disease risk, BMI, blood pressure, hemoglobin, bood glucose, physical activity; C: depression, perceived stress, sleepiness. |
Age, sex, race |
- Irregularity ~ +age, female, Caucasian ethnicity, employment status, +daily light exposure (small), +risk for cardiovascular disease (small-moderate), +blood pressure (small), +BMI (small), +serum hemoglobin (small), +blood glucose (small), -physical activity (small), +depression, +perceived stress, +eveningness (small); +sleepiness (moderate); NS for education.
|
|
Medeiros et al.
|
2001 |
Observational |
Questionnaire and objective academic performance data examined along 2-week sleep diary. |
36 Com (medical students) |
NR (BR) |
20.7(2.2) |
42% |
14 |
Diary |
ISD |
|
C: Chronotype, academic performance. |
None. |
SOTv ~ +evening chronotype, -academic performance. |
|
Chan
|
2017 |
Observational |
7 d actigraphy and diary, followed by computerized tasks and self-reported sleepiness and hunger self-reports. |
78 Uni |
76% White, 11% Black, 9% Asian, 3% Latino |
20.38 (2.40) |
56.0% |
7 |
Actigraphy (with Diary) |
ISD |
B, C |
B: BMI;
C: delay discounting, response inhibition |
Perceived stress, physical activity, daytime nap duration, alcohol/caffeine |
- BTv ~ +BMI controlling for covariates;
- RTv ~ +BMI, NS controlling for covariates;
- Delay discounting moderated BMI ~ BT, BTv, TSTv, RTv; associations significant in high delay discounting rate. Response disinhibition moderated BMI ~ BTv; similar pattern.
|
|
Phillips et al
|
2017 |
Observational |
Campus housing. 30 d diary; on day 15, highest and lowest sleep regularity index (12 each) completed actigraphy and DLMO. |
24 Uni (full sample 61) |
87% White, 10% Asian, 2% Black, 1% Hawaiian/Pacific Islander |
20.23 (1.27) |
47.54% |
30 and 15 |
Actigraphy (with Diary) |
Sleep Regularity Index (SRI): average % of being in the same state (sleep vs wake) at any 2 time points 24 h apart |
A, B, C |
A: light exposure;
B: DLMO;
C: GPA |
Respective means of sleep variables |
- High SRI (regular) ~ +TSTm (10pm-10am), -TST (10am-10pm), earlier and more variable SOT and RT, -Nap, earlier peak of sleep propensity rhythm; +light/dark cycle amplitude, +day light, +broader range of light-exposure centroid times; later DLMO; +GPA (moderate).
- TSTm ~ SRI NS;
|
|
Chan et al
|
2017 |
Intervention |
2 w BL, 4 w weekly CBT-I or Ctrl, 2 w POST, 2 w 3-m FU. |
62 Insomnia (older) |
82.26% White, 6.45% Hispanic, 3.23% Black, 3.23% Asian, 4.84% Other. |
69.45 (7.71) |
67.74% |
14 for BL, POST, FU, 28 for treatment. |
Actigraphy and Diary |
ISD |
A, D |
A: Education; D: Effects of CBT-I |
Respective means of sleep variables, insomnia duration, education, sleep medications. |
- CBT-I ~ +reductions in Diary SOLv and actigraphy TSTv, but not Nap;
- Above effects mediated by reductions in BTv, RTv, TIBm;
- Time x group x BL sleepv interaction sig: BL sleepv ~ +treatment response;
- BL SOLv, TSTv, SEv ~ +likelihood of taking sleep medication;
- BL SOLv ~ - lower education.
|
|
Bernert et al
|
2017 |
Observational |
3 time points with questionnaires; actigraphy and diary at T1 (1w) and T2 (2w). |
50 Uni with suicide attempt history and recent ideation |
74% White, 12% Hispanic, 6% Black, 2% Asian, 4% Mixed, 2% Other |
19.2 (1.4) |
72.0% |
7 and 14 |
Actigraphy (with Diary) |
ISD |
A, C, D |
A: Shiftwork;
C: Suicidal ideation;
D: Insomnia |
T1 suicide ideation, depressive symptoms, alcohol-related problems. |
- Sleep timing v ~ shiftwork;
- SOTv ~ +change in suicidal ideation T2 to T3;
- Sleep v ~ T2 insomnia (moderate).
|
|
Burgess et al
|
2017 |
Observational |
10 d protocol: DLMO on 2 nights both before and after a 5 d break |
40 (22 DSWPD, 18 healthy) |
67.5% White, 7.5% Black, 12.5% Asian, 12.5% Other |
DSWPD: 28.0 (7.2); Ctrl: 30.8 (7.3); |
45.0% |
5 |
Actigraphy (with Diary) |
RMSSD |
A, B, D |
A: morning commitments, weekday weekend difference;
B: shift in DLMO;
D: DSWPD status |
None. |
- NS weekday-weekend difference in RMSSD for all sleep variables in either group;
- Sleep v and morning commitments: NS;
- DSWPD ~ +RTv, +TSTv, SEv and SOLv NS;
- SOTv ~ + shift in the DLMO, but only in DSWPD.
|
|
Bei et al
|
2017 |
Observational |
7 d actigraphy and in-lab physiological measures. |
436 Com |
70.1% White, 28.0% Black, 1.8% Other |
54.1 (11.7) |
60.3% |
7 |
Actigraphy (with Diary) |
Bayesian IIV model |
B |
B: allostatic load (AL) and individual system not accounted for by AL, cortisol trajectory |
Respective means of sleep variables. Cortisol models: age, sex, race, education, bed partner, smoking, perceived stress, chronic major medical conditions. AL analyses: age, sex, race, smoking, perceived stress, chronic major medical conditions, AL relevant medications. |
- Cortisol: flatter diurnal slope ~ +BTv (trend), +RTv, +TSTv; - awakening cortisol ~ +RTv (trend);
- AL: controlling for age and sex: higher AL ~ +SOLv, +WASOv, +BTv (trend); these NS after controlling for other covariates.
|
|
Cohen et al
|
2017 |
Observational |
Daily sleep and behavioural observations at residential facilities. |
67 low-functioning autism. |
88% White, 4.5% Hispanic, 4.5% Asian, 2.9% Native American |
13.29 (3.06) |
20.0% |
Average 306 (48–534). |
Caretakers observation every 15 or 30 min. |
SRI |
C |
C: Challenging behaviour, aggression, self-injury, tantrums, property destruction |
None. |
- Prior days' sleep predicting outcomes was most strongly driven by TSTv and nighttime wakening variability;
- Significant predictive relationship in 81% of individuals.
|
|
Chung
|
2017 |
Observational |
Actigraphy and diary study. |
236 Com |
NR (US) |
53.61 (11.67) |
56.36% |
7 |
Actigraphy and Diary |
Log-transformed MSSD |
C |
C: Social support, social strain |
Self-rated health, dyspnea, chronic conditions, depression, age, sex, marital status, exercise, caffeine, alcoholic drinks. |
- TSTv ~ + social strain but NS with social support.
|
|
Kanady et al
|
2017 |
Intervention |
RCT comparing CBT-I and psychoeducation Ctrl; both 8 weekly sessions. |
66 Bipolar Disorder; 47 with and 19 without comorbid insomnia diagnosis; 20 completed CBT-I, 18 completed Ctrl. |
Comorbid insomnia: 66.67% White, 11.11% Black, 9.26% Asian, remaining Other; Ctrl: 52.17% White, 13.04% Black, 4.35% Asian, remaining Other. |
Comorbid insomnia: 36.76 (11.23); Ctrl: 30.74 (10.06) |
Comorbid insomnia: 63.0%; Ctrl: 65.2% |
7 |
Diary |
RMSSD |
C, D |
C: Working memory, verbal learning;
D: Effects of CBT-I. |
Age. |
- BL TSTv ~ -verbal learning, working memory performance, independent of insomnia diagnosis;
- Sig Group x TSTv interaction: in CBT-I group, reductions in TSTv ~ improved verbal learning (moderate).
|
|
Breneman et al
|
2017 |
Intervention |
RCT on low vs high-dose exercises of 4 m; actigraphy at BL, mid-intervention (MID), POST. |
49 healthy, physically inactive older women. |
83.67% White, 14.29% Black, 2.04% Other |
64.53 (3.83) |
100% |
7 at BL, MID, POST |
Actigraphy (with Diary) |
ISD, CV |
B |
B: cardiorespiratory fitness (VO₂peak), effects of exercise intervention. |
Mixed-effects model. |
- Main effect of time: WASOv lower at MID and POST compared to BL, but MID vs POST NS; NS for other sleep variables;
- Using ISD: BL VO₂peak ~ -TSTv, -WASOv; Using CV, BL VO₂peak ~ -TSTv but not WASOv.
|
|
Caia et al
|
2017 |
Observational |
7 d actigraphy and diary in March (first month of competitive season). |
45 Australian rugby athletes. |
NR (AU) |
15 elite seniors: 25.5 (3.7), 15 sub-elite seniors: 22.4 (2.4), 15 elite juniors: 18.8 (0.9) |
NR |
7 |
Actigraphy (with Diary) |
ISD |
A, B |
A: Age; B: Elite vs sub-elite |
None. |
Compared to seniors, juniors ~ +SOLv, +TIBv, +TSTv, +Qulityv.
|
|
Diem et al
|
2016 |
Observational |
Daily Actigraphy and Diary; other cognitive and health measures. |
1245 women without dementia |
NR (THAI) |
82.6 (3.3) |
100% |
Minimum 3 d |
Actigraphy (with Diary) |
ISD and quartile |
A, C |
A: age;
C: Risk for mild cognitive impairment (MCI) and dementia |
Minimally adjusted: age, race, clinic, education. Multivariate adjusted: aforementioned, BMI, depression, comorbidities, functional impairments, smoking, alcohol, exercise, living alone, health status, antidepressant, benzodiazepine, sleep medication. |
- TSTv and SEv ~ +risk of MCI and dementia after full adjustments;
- WASOv and SOLv NS.
|
|
Ogilvie et al
|
2016 |
Observational |
7 d actigraphy and diary; cross-sectional health measures |
2146 older |
NR (US) |
68.6 (9.2) |
53.7% |
7 |
Actigraphy (with Diary) |
ISD |
A, B |
A: age, sex, race
B: BMI, waist circumference, body fat |
M1: age, sex, race, field center; M2: M1 plus depressive symptoms, anti-depressants, alcohol, sleep medication, smoking, income, marital status, education; M3: M2 plus sleep apnea; M4: M3 + sleep duration |
- TSTv ~ +BMI, +waist circumference, +body fat. NS controlling for demographics and TST (i.e., M4);
- NS interactions by race, age, or sex;
- Highest quartile TSTv had % obesity.
|
|
Aubin et al.
|
2016 |
Observational |
Between group comparisons on 30 D sleep |
11 blind, 11 controls |
NR (DK) |
44.5 (14.9) |
63.64% |
10 |
Actigraphy (with Diary) |
Range |
B, C |
B: Blindness;
C: Chronotype |
None. |
- SEv and Sleep Offset v: Blind > Control.
- SOT: NS between group.
- Sleep on/offset timing variability and chronotype: NS.
|
|
Kaufmann et al.
|
2016 |
Observational |
Ecological Momentary Assessments over 11 W |
41 outpatients with Bipolar I & II |
78% White, 9.8% African-American, 12.2% Other |
46.9 (11.8) |
53.70% |
77 |
Diary |
ISD and daily "atypicality" (each subject's current day TST minus TSTm then squared). |
A, C |
A: Age, sex, race, education;
C: Daily mood |
None. |
- TSTv ~ -age (NS with sex, race, education); + symptom severity; - medication adherence; + variability of daily energy, sadness, & impulsivity; mean anger, anxiety, stress, & impulsivity.
- Daily TST atypicality ~ - same day energy, + same day sadness, - anxiety in 2 days; NS for other outcomes
|
|
Tsai et al.
|
2016 |
Observational |
Poor vs good sleepers (based on PSQI) |
197 first-time mothers in 3rd trimester |
NR (TW) |
31.98 (4.21) |
100% |
7 |
Actigraphy (with Diary) |
ISD |
D |
D: Sleep complaints |
None. |
- TSTv, SOLv, WASOv: Poor > Good sleepers.
|
|
Lee S et al.
|
2016 |
Intervention |
7 D actigraphy at BL and 1 Y FU after a 3 M workplace intervention. |
396 IT employees |
73.7% White, 16.2% Asian or Pacific Islander |
46.97 (8.45) |
41% |
7 BL, 7 FU |
Actigraphy |
Within-person variance in multilevel models. |
A |
A: Age; workplace intervention |
Means of sleep variables. |
- Sig interaction for Age x Intervention x Time for WASOv and Napv: + age and receiving intervention ~ + reduction in FU WASOv;
- age and receiving intervention ~ + increase in Napv.
- Age x Intervention x Time NS for TSTv.
|
|
Cespedes et al.
|
2016 |
Observational |
7 D actigraphy naturalistic observation |
2086 Hispanics/Latinos |
100% Hispanics/Latinos |
47.1 (11.5) |
64.77% |
7 |
Actigraphy (with Diary) |
ISD; top quartile (SD > 1.5hrs) considered high IIV |
C/D |
C/D: Self-report vs actigraphy sleep duration |
None. |
- High TSTv ~ weaker associations between self-reported vs actigraphy TST.
|
|
Ong et al.
|
2016 |
Intervention |
3-arm RCT: MBSR, MBTI, self-monitoring CTRL; daily diary for BL (1 w), EARLY (2 w), LATE (6 w), and POST intervention. |
54 Insomnia |
NR (US) |
42.9 |
74.10% |
7 BL, 14 EARLY, 42 LATE, and 7 POST intervention |
Diary |
Location-scale mixed model |
D |
D: Treatment-related changes in SE |
SEm |
- Simple effects on SEv: MBSR had +reduction at EARLY, LATE, and POST; MBTI had +reduction at LATE and POST but not EARLY.
- Compared to CTRL: MBSR had +reduction in SEv from BL to EARLY and LATE (30%), but not to POST; NS. b/w MBTI and CTRL.
- Compared to MBTI, MBSR had +reduction in SEv from BL to EARLY (but not to LATE or POST).
|
|
Ng et al.
|
2016 |
Observational |
7 d sleep diary and self-report questionnaires |
84 patients with Bipolar Disorder |
100% Chinese |
44.04 (10.49) |
67.86% |
7 |
Diary |
Multilevel modeling of square successive difference |
A, C |
A: Age;
C: Social rhythm, chronotype, DBAS, sleep hygiene, major depression occurrence, type of Bipolar Disorder, depressive symptoms, mania severity. |
None |
- TSTv ~ -social rhythm regularity, +major depression past 5 years;
- SOLv and SEv ~ -social rhythm regularity;
- WASOv ~ +DBAS, onset of major depression at 2 year follow-up;
- Other factors NS related to any sleepv variables: age, Bipolar I or II, mania severity, depressive symptoms.
|
|
Chontong et al.
|
2016 |
Observational |
5 d actigraphy and medical records extraction for correlates |
41 patients with type 1 diabetes, stable insulin regimen |
NR (THAI) |
41.5 (14.8) |
61% |
5 |
Actigraphy with Diary |
ISD |
B, C |
B: HbA1c, insulin requirement;
C: depressive symptoms. |
Neuropathic symptoms, OSA risk, self-reported sleep quality |
- Both SMv and TSTv ~ +HbA1c;
- High vs Low TSTv groups: High group had higher HbA1c, and higher required insulin (NS for diabetes complication or depressive symptoms).
|
|
Whiting & Murdock
|
2016 |
Observational |
7 d actigraphy before in-lab cognitive tests |
81 Uni |
87% White, 10% Asian |
20.54 (1.22) |
57.80% |
3 |
Actigraphy with Diary |
ISD |
C |
C: Attentional capture |
Means of sleep variables |
- Variable sleep interval duration ~ - attentional capture, especially for those with short sleep duration;
- NS findings for SOTv and WTv.
|
|
Baron et al.
|
2016 |
Intervention |
1 w BL , 16 w sleep hygiene with or without exercise interventions; associations between sleep variability and outcomes assessed at BL. |
17 Insomnia (older, short TST) |
NR (US) |
61.6 (4.3) |
94.10% |
7 for BL, 112 for Intervention |
Actigraphy |
ISD |
B |
B: Cardiometabolic disease risk (HbA1c, BMI, fasting glucose, fasting insulin, HOMA, OGTT, presleep cortisol, CRP) |
Age, means of sleep variables |
- TSTv ~ +HbA1c, SOTv ~ +BMI;
- Fasting glucose, fasting insulin, HOMA, OGTT, presleep cortisol, CRP NS with sleep variability;
- WASOv & SEv: BL > POST, but NS for TIBv, TSTv, SOTv, WTv, SOLv, Fragmentationv.
|
|
Taylor et al.
|
2016 |
Observational |
14 d self-report sleep, PSG sleep, and other health
measures cross-sectionally at T1; health also measured
in 5.4 y (T2) |
338 Com |
47.6% White, 35.8% Black, 16.5% Asian |
52.12 (2.10) |
100% |
14 |
Diary |
ISD |
B |
B: BMI, HOMA-IR |
BTm, TSTm, race, menopausal status, exercise,
depressive symptoms; T1 values in T2 analyses; BMI in
HOMA-IR analyses. |
- T1 BTv ~ +BMI (but NS after controlling for
covariates) for both T1 & T2;
- T1 BTv ~ +HOMA-IR (with/without covariates)
at T1 but not T2.
|
|
Shoji et al.
|
2015 |
Observational |
14 d self-report pre-sleep arousal and sleep, Young
vs Old. |
50 older & 50 younger Com |
Young: 70% White, Old: 90% White |
Young: 19.88 (2.76); Old: 67.81 (6.73) |
Young: 72%; Old: 60% |
14 |
Diary |
ISD after detrending; interclass correlations |
A |
A: Age |
None |
- % of within- vs b/t person variability:
Young > Old (SOL, WASO, TST, SQ, Pre-sleep
Arousal);
- TSTv, WASOv, SQv: Young > Old;
- SOLv, Pre-sleep arousal IIV: NS.
|
|
Moss et al.
|
2015 |
Observational |
2 w self-report, Insomnia vs Healthy |
33 Insomnia, 36 Healthy |
Insomnia: 79% White, Healthy: 52% White |
Insomina: 47 (12), Healthy 32 (13) |
Insomina: 76%, Healthy: 73% |
14 |
Diary (SRM) |
ISD |
D |
D: Insomnia |
Age |
BTv & RTv: Insomnia > Healthy |
|
Kim et al.
|
2015 |
Observational |
9 d Actigraphy and body composition via X-ray
absorptiometry |
191 Com (Old) |
100% Japanese |
83.4 (2.6) |
100% |
9 |
Actigraphy |
ISD for sleep variables; principle component
analysis for "Inconsistent sleep/wake patterns" |
B |
B: Body composition |
TSTm, Napm, age, education, living alone, alcohol,
smoking, Nr chorionic diseases, sleep medication,
cognitive function, depression, self-reported health,
sleep nights, physical activity. |
- Inconsistent sleep ~ +BMI, +%fat, +FMI,
-%lean, -lean/fat ratio;
- BTv ~ +BMI, +%fat, +FMI, -%lean, -lean/fat
ratio; RTv & SMv: NS;
- TSTv ~ +%fat, +FMI, -%lean, -lean/fat
ratio; BMI: NS.
|
|
Straus et al.
|
2015 |
Observational |
Questionnaire, 1 w Actigraphy & Diary, PTSD vs
Insomnia vs Healthy |
45 PTSD, 25 Insomnia, 27 Healthy |
70.1% White |
33.51 (8.26) |
23.70% |
7 |
Actigraphy & Diary |
RMSSD |
C, D |
C: PTSD
D: Insomnia |
None |
- Actigraphy & Diary TSTv, WASOv, SEv, Diary
SOLv: PTSD & Insomnia both > Healthy;
- Actigraphy SEv & Diary TSTv: PTSD >
Insomnia; other variables NS b/w PTSD &
Insomnia.
|
|
Ankers & Jones
|
2009 |
Observational |
Hypomanic risk vs Ctrl. |
55 Uni |
NR (UK) |
21.44 (3.36) |
70.9% |
7 |
Actigraphy & Diary |
ISD |
C |
C: Risk of hypomania (bipolar). |
Internal state, hypomanic interpretation |
- BTv & RTv: hypomanic risk group > Ctrl;
BTv predicted group membership controlling for
covariates;
- TSTv: hypomanic risk group > Ctrl;
- SEv & Fragmentation: hypomanic risk group
> Ctrl; SOLv & %WASO: NS b/w groups.
|
|
Ari & Shulman
|
2012 |
Observational |
2 time points in 1st & 2nd academic semesters. |
150 Uni |
88.2% Isreali |
22.99 (1.75) |
76.4% |
7 |
Diary |
Average difference from mean. |
C |
C: Adjustment to college. |
None |
TSTv: low at both times in well-adjusted group;
high in 1st low in 2nd semester in re-adjusted
group. |
|
Bijlenga et al.
|
2013 |
Observational |
Pts vs Ctrl |
24 ADHD & DSPD vs. Ctrl |
NR (NL) |
32.4 (10.1) |
50.0% |
5 |
Diary |
Variance |
C |
C: Comorbid ADHD & DSPD. |
None |
SOTv: ADHD & DSPD > Ctrl. |
|
Bliwise et al.
|
2005 |
Observational |
2 time points 10 years apart. |
31 Com |
NR (US) |
66.5 (8.0) |
67.7% |
14 & 7 |
Diary |
Variance |
A, B |
A: Age, cohabitation;
B: Onset of physical illness. |
None |
- BTv & RTv: NS differences b/w T1 & T2 (with
or without physical illness onset b/w time
points); Cohabitation with -BTv & -RTv at
T2.
- Napv: NS difference b/w T1 & T2.
|
|
Bonnet & Alter
|
1982 |
Experimental |
2W BL, 38 days regular sleep in lab, 4W habitual
sleep, 2W FU. |
12 Uni |
NR (US) |
19-28 |
0.0% |
14 for BL FU, 7 for manipulation. |
Diary |
ISD |
C, E |
C: Mood, vigilance, body temperature, momentary
arousal. |
None |
- BTv, RTv, TSTv: regular < irregular
conditions;
- Mood, cognitive performance, sleep
architecture: NS regular vs irregular
conditions;
- Body temperature: regular < irregular
conditions.
|
|
Buman et al.
|
2011 |
Intervention |
RCT for sleep complaint, Exercise vs health
education Ctrl. |
36 Com |
92% White |
61.42 (6.72) |
NR |
14 BL, 7 at 6 & 12 months after BL. |
Diary |
CV |
D |
D: Exercise for sleep complaints. |
None |
- BTv & RTv: NS b/w Exercise & Ctrl;
- TIBv: Exercise < Ctrl at 6 months
(moderate);
- SOLv: Exercise < Ctrl at 12 months
(moderate);
- nWASOv: NS b/w Exercise & Ctrl.
|
|
Buysse et al.
|
2010 |
Observational |
Insomnia (chronic) vs Ctrl (healthy). |
92 Com (older) |
95.6% White |
71.16 |
66.3% |
14 |
Actigraphy & Diary |
ISD & mixed model |
C, D |
C: Depressive symptoms;
D: Insomnia symptoms. |
None |
- BTv: Insomnia < Ctrl; RTv: Insomnia >
Ctrl;
- TIBv: NS Insomnia vs Ctrl; TSTv: Insomnia
> Ctrl on Diary, NS on Actigraphy;
- SEv & WASOv: Insomnia > Ctrl (Diary &
Actigraphy); SOLv: Insomnia > Ctrl on Diary,
NS on Actigraphy; Qualityv: Insomnia >
Ctrl.
- Insomnia group: only TIBv ~ +depressive
symptoms, weak relationship b/w Diary IIV &
sleep quality, sleepiness, or depressive
symptoms.
|
|
Carney et al.
|
2006 |
Observational |
Good vs Poor sleepers based on PSQI. |
243 Uni |
79% White, 14% Black |
20.98 (3.24) |
87.9% |
14 |
Diary (SRM) |
ISD |
D |
D: Good vs Poor sleep. |
Depressive symptoms. |
- BTv: Poor >Good sleepers, NS after
controlling for depressive symptoms;
- RTv: Poor > Good sleepers with/without
controlling for depressive symptoms.
|
|
Cheek et al.
|
2004 |
Observational |
Women with insomnia vs healthy Ctrl. |
121 Com |
80% White |
46.57 (4.07) |
100.0% |
5 |
Diary & PSG initiation/termination |
ISD |
D |
D: Insomnia symptoms |
Age |
- BTv ~ -sleep quality;
- SOLv: Insomnia > Ctrl; WASOv: NS b/w
Insomnia & Ctrl; Qualityv: Insomnia >
Ctrl.
|
|
Dautovich et al.
|
2012 |
Observational |
Naturalistic observation. |
103 Com (older) |
96.1% White |
72.90 (6.86) |
64.1% |
14 |
Actigraphy & Diary |
ISD after detrending based on the whole sample |
B |
B: Self-report Nr. health conditions |
Age |
Napv (Diary not Actigraphy): +Nr health
conditions. |
|
Dillon et al.
|
2014 |
Observational |
Naturalistic observation. |
592 Normal sleepers |
70.1% White, 29.9% Black |
52.3 (19.5) |
50.3% |
14 |
Diary |
ISD & multilevel modeling |
A, C |
A: Age;
C: Depressive symptoms. |
Mean values, age, sex, race, depressive
symptoms. |
- TSTv: ~ +depressive symptoms, -age, age x
sex, sex x race, age x sex x race (all
small);
- SOLv: ~ +SOLm (large), -age (small),
+female (small), black race (small);
- nWASOv: +nWASOm (large), +education
(small), -age (small), +female (small); WASOv:
+WASOm (large), -age (small);
- Within-person variability > b/w-person
variability.
|
|
Edinger et al.
|
1992 |
Intervention |
2, 4, or 6W BL, 4W relaxation therapy, 2W
assessment, 4W CBT, 2W assessment, 3-month FU. |
7 Insomnia (sleep maintenance) |
100% White |
61.9 (55-68) |
57.1% |
14 for Diary, 7 for SAD |
Diary & SAD |
ISD |
D |
D: Insomnia intervention |
None |
- TIBv & TSTv: decreased over time on Diary,
NS change on SAD;
- SEv: decreased over time on both Diary &
SAD;
- SOLv: decreased over time on dairy, NS on
SAD;
- nWASOv: NS change over time on Diary;
decreased after CBT on SAD, WASOv decreased
over time;
- Qualityv: NS change over time on
Diary;
- Napv: NS change over time.
- Multivariate analyses: intervention reduced
overall variability on both Diary & SAD. Most
changes occurred after CBT but not after
RT.
|
|
Eidelman et al.
|
2010 |
Observational |
Naturalistic observation of IIV followed by
interviews & questionnaires. |
21 Inter-episode bipolar Pts |
71.4% White |
37.0 (10.65) |
85.7% |
7 |
Diary |
ISD |
C |
C: Bipolar age of onset, lifetime manic/depressive
episodes, manic/depressive symptoms. |
None |
- BTv: NS for all correlates (but moderate ~
+depressive episodes);
- SOTv: ~ +depressive symptoms (large), NS ~
other correlates;
- TSTv: NS ~ all correlates;
- SEv: ~ +depressive episodes (large), NS ~
other correlates;
- WASOv: ~ +depressive episode (large), NS ~
manic episodes (but moderate), NS ~ other
correlates.
|
|
Espie et al.
|
1989 |
Intervention |
RCT of 8W relaxation, stimulus control, paradoxical
intention, imagery relief placebo, or no treatment. 2W
BL, assessments at 6W, 3, 6, & 17 months FU. |
70 Insomnia (sleep onset) |
NR (UK) |
44.9 (15.3) |
67.1% |
14 for BL, 7 for other assessments |
Diary with SAD |
ISD |
D |
D: Insomnia symptoms |
None |
- TSTv: ~ -time, NS treatment effect,
significant treatment x time effect;
- SOLv: ~ -time, -treatment, significant
treatment x time effect;
- Only active treatment improved sleep.
Stimulus control improved sleep patterns,
relaxation improved perceived sleep quality.
Most results maintained at all FU.
|
|
Fainstein et al.
|
1997 |
Intervention |
3 groups with sleep disturbance: with depression,
with dementia, with neither. Compared day start & end
IIV on 21-day melatonin treatment. |
41 Insomnia |
NR (AR) |
74 (12) |
68.3% |
3 |
Diary |
CV |
C, D |
C: Cognitive & psychiatric comorbidity;
D: Sleep intervention. |
None |
BTv: significant decrease in dementia but not other
two groups. |
|
Fichten et al.
|
2005 |
Observational |
3 groups of poor (research criteria insomnia),
medium, good sleeper. |
148 Com (older) |
NR (CA) |
69 (55-87) |
65.5% |
7 |
Diary |
ISD |
D |
D: Good vs poor sleepers & their estimation of
time. |
None |
- TSTv: NS group differences;
- SOLv: poor sleepers > other groups;
- WASOv: poor sleepers > other
groups;
- Poor sleepers more variable in wake
(SOL+WASO), yet this does little to explain
their biased perception of own sleep
problems.
|
|
Geoffroy et al.
|
2014 |
Observational |
Bipolar in remission vs healthy Ctrl matched on age
& sex. |
55 Bipolar & Ctrl |
NR (FR) |
53.82 (10.30) |
54.5% |
21 |
Actigraphy (with Diary) |
ISD |
C |
C: Bipolar in remission |
None |
- TIBv & TSTv: Bipolar remission >
Ctrl;
- SEv: Bipolar remission > Ctrl;
- SOLv: NS group differences;
- WASOv: Bipolar remission > (trend)
Ctrl;
- Fragmentationv: Bipolar remission >
Ctrl;
- TSTm, SOLm, Fragmentationv, PSQI daytime
function correctly classified 89% of study
participants as cases or controls.
|
|
Hauri & Wisbey
|
1992 |
Observational |
1W home Actigraphy then 3 days lab Actigraphy with
≥6hrs TIB. |
36 Insomnia |
NR (US) |
45 (24-69) |
63.9% |
7 at home 3 in lab |
Actigraphy |
ISD |
A |
A: Home vs lab setting in insomnia |
None |
TSTv: home > lab. |
|
Hayes et al.
|
2014 |
Observational |
3 groups of aMCI, non-aMCI, & "Intact". |
45 Com (older) |
NR (US) |
86.9 (4.3) |
88.9% |
182 |
Movement based bed mats (validated against
Actigraphy) |
Inter-quartile range |
C |
C: Cognitive function |
None |
- WASOv: aMCI < Intact or naMCI;
- non-aMCI showed sleep disturbance that was
intermediate to that of aMCI & intact.
|
|
Hoaki et al.
|
2011 |
Observational |
1W Actigraphy & questionnaires. |
56 Healthy |
NR (JP) |
26.9 (5.9) |
30.4% |
7 |
Actigraphy |
ISD |
C |
C: Hyperthymic temperament (bipolar) |
Daytime illuminance, ACTH |
TSTv: NS correlation with hyperthymic temperament,
but ~ +hyperthymic temperament when controlling for
covariates. |
|
Innes et al.
|
2013 |
Observational |
1W BL, then 1 night sleep restriction to 4 hrs,
then normal sleep. |
16 Healthy |
NR (NZ) |
24.9 (20-37) |
50.0% |
6 |
Actigraphy (with Diary) |
ISD |
C |
C: Microsleep after sleep restriction |
None |
SOTv of BL: ~ -number of microsleeps following
sleep restriction (large). |
|
Kang & Chen
|
2009 |
Observational |
2W Diary followed by assessments. |
160 Uni |
100% Chinese |
20.3 (1.9) |
49.4% |
14 |
Diary |
Nr of nights/W with >1hr shift in BT: low
(<1), intermediate (1-3), high (>3). |
C |
C: Subjective sleep, fatigue, sleepiness. |
TSTm |
- 26.9% low, 38.8% intermediate, 34.4%
high.
- BTv: with poorer subjective sleep (large,
more so in intermediate & high groups); NS ~
fatigue or sleepiness.
|
|
Khawaja et al.
|
2013 |
Observational |
2W Actigraphy with questionnaires. |
23 Veteran with PTSD & sleep disturbance |
NR (US) |
52.8 (10.3) |
13.0% |
14 |
Actigraphy |
ISD |
A, C |
A: Age;
C: PTSD. |
nWASOm |
nWASOv: ~ -age (large), -TSTm (large). |
|
Knutson et al.
|
2007 |
Observational |
3 days’ Actigraphy, twice ~1 year apart. |
669 Com |
44% Black |
42.9 (3.7) |
57.0% |
3 |
Actigraphy (with Diary) |
Custom formula |
A |
A: Race, daily vs yearly |
Age, race, sex, weekend |
TIBv, TSTv, SEv, SOLv: daily IIV > yearly IIV;
black > white. |
|
Kramer et al.
|
1999 |
Observational |
2W Diary & Actigraphy in Older vs Younger. |
21 (Older) & 19 (Younger) Healthy |
NR (NL) |
65.1 (4.4) & 20.8 (2.2) |
0.0% |
14 |
Diary |
ISD |
A |
A: Age |
None |
- BTv: Younger > Older;
- RTv: Younger > Older.
|
|
Kubo et al.
|
2009 |
Observational |
1W home Diary (no naps/sleep
deprivation/caffeine/alcohol); 9 days lab (Day 1
adaptation, Day 2 BL, 4 days simulated night shift, 3
days simulated day shift). |
10 Healthy |
NR (JP) |
22.9 (3.2) |
0.0% |
7 |
Diary |
ISD |
C |
C: Recovery pattern from simulated shift
schedules |
None |
Recovery patterns related to home BTv (moderate),
RTv (large), but not to alertness & performance during
the simulated night shifts. |
|
Lemola et al.
|
2013 |
Observational |
1W home Actigraphy with Diary. |
441 Com |
66.6% White, 33.3% Black |
56.85 (11.38) |
60.4% |
7 |
Actigraphy (with Diary) |
CV |
C |
SWL, psychological distress. |
Gender, age, marital status, education, BMI,
ethnicity, twin status. |
TSTv: black >white; M < F in black; ~ -SWL,
+distress (i.e., mood & anxiety). |
|
Manber et al.
|
1996 |
Experimental |
12 days BL, 4W natural vs regular sleep
manipulation within 1hr window of habitual sleep timing
(all asked to sleep ≥7.5hrs, light & activity upon
awakening, minimize coffee), FU at 5W post for 1W |
39 Uni (sleepy & irregular) |
NR (US) |
18.8 (0.97) |
69.2% |
7 |
Diary |
ISD |
C, D, E |
C: Daytime sleepiness;
D: Sleep quality. |
None |
- Good compliance with manipulation for
regular vs natural conditions.
- BTv: ~ +sleepiness at BL;
- SEm increased & SOLm decreased in regular
but not natural group; NS differences in
WASOm;
- When not sleep deprived, regular group had
greater & longer lasting reduction in daytime
sleepiness.
|
|
McBean & Montgomery-Downs
|
2013 |
Observational |
From beginning of 2nd postpartum week, PVT every
morning for 12W. |
71 Healthy (primiparas) |
90.1% White |
26.3 (4.1) |
100.0% |
7 |
Actigraphy & Diary |
ISD |
B, C |
B: Time since giving birth;
C: PVT, daytime function. |
Age |
SMv: NS change across W2-W12; SMv at W2 ~ +PVT
lapses at W2, W5-W13; NS ~ slope of change in PVT
lapses over time; SMv ~ +daytime impairments. |
|
McCrae et al.
|
2006 |
Observational |
4 groups: with/without insomnia by complaint vs no
complaint. |
Sample 1: 310, Sample 2: 103, Com (older) |
Sample 1: 77.7% White, 22.0% Black; Sample 2:
NR |
60-96 |
Sample 1: 51.3%, Sample 2: NR |
14 |
Diary |
ISD |
D |
D: Insomnia & sleep complaints |
Age, education, sex, medications, health
conditions |
BTv & RTv: NS group differences. |
|
McCrae et al.
|
2012 |
Observational |
2W Diary. |
72 Com (older) |
“Mostly” White |
70.18 (7.09) |
66.7% |
14 |
Diary |
ISD |
C |
C: Cognitive function (inductive reasoning,
processing speed) |
Age, education, complaint duration |
TSTv & TWTv: NS ~ inductive reasoning or processing
speed. |
|
Merklinger-Gruchala et al.
|
2008 |
Observational |
daily self-report of TST over menstrual cycle. |
95 Com |
100% Polish |
29.48 (3.13) |
100.0% |
28.88 (3.83) |
Diary |
CV |
A, B |
A: Age, education, duration of daylight;
B: Estradiol levels etc (see results). |
TSTm |
TSTv: ~ +estradiol; NS ~ age, birth weight,
education, energy intake, physical activity,
weight/height, body fat, BMI, age at menarche, length
of menstrual cycle during collection, mean duration of
daylight. |
|
Meyer & Maier
|
2006 |
Observational |
4W SRM, comparing bipolar risk, unipolar risk, &
Ctrl. |
141 Uni |
100% native German speaker |
18.18 (2.14) |
70.7% |
28 |
SRM |
ISD |
C |
C: Risk for bipolar & unipolar. |
None |
TSTv: bipolar risk > both unipolar risk & Ctrl;
NS b/w Ctrl & unipolar risk; results hold excluding
those with unipolar or bipolar disorder. |
|
Mezick et al.
|
2009 |
Observational |
9 days Actigraphy, norepinephrine from overnight
urine on nights 2 & 4. |
184 Com |
57.1% White, 40.8% Black |
59.5 (7.2) |
47.3% |
9 |
Actigraphy |
ISD |
A, C |
A: Race, sex;
C: Stress; |
Sex, race, age, BMI, apnea-hypopnea index,
medication use, & the relevant mean |
- TSTv: NS b/w black & white, F > M; ~
+stressful life events, NS ~
norepinephrine.
- Fragmentationv: black > white; NS b/w
sexes.
- NA as moderator: in those with higher NA,
Fragmentationv (but not TSTv) ~ +stressful life
events, greater TSTv & Fragmantationv ~
+norepinephrine.
|
|
Millar et al.
|
2004 |
Observational |
Remitted bipolar I patients vs age gender matched
Ctrl. |
38 remitted bipolar & Ctrl |
NR (UK) |
46.55 (10.77) |
57.9% |
5 |
Actigraphy & Diary |
ISD |
C |
C: Remitted bipolar pts vs Ctrl |
Daily mood ratings |
- Actigraphy: NS group difference on TSTv,
SOLv, SEv, WASOv (multivariate); remitted
bipolar > Ctrl: TSTv & WASOv
(univariate);
- Diary: remitted bipolar > Ctrl: TSTv,
SOLv, SEv, WASOv (multivariate); remitted
bipolar > Ctrl: TSTv, SOLv, & SEv
(univariate);
- Best group membership model: Actigraphy
TSTv, Diary TSTm, Diary SOLm.
|
|
Minors et al.
|
1998 |
Observational |
Diary during "typical week", comparisons of data 10
years apart. |
112 Com (older) |
NR (UK) |
73.00 |
80.0% |
7 |
Diary |
Variance |
A |
A: Age, sex, cohabitation |
sex |
- BTv: T1 > T2 (NS trend) in cohabitation,
NS for living alone;
- RTv: T1 > T2 in cohabitation, NS for
living alone;
- TIBv: T1 > T2 in cohabitation, NS for
living alone;
- Napv: ~ +cohabitation at T1 but not T2; NS
change b/w two times.
- All above variables ~ -age at T1 but not
T2; NS ~ sex.
|
|
Monk et al.
|
1991 |
Observational |
2W Diary. |
34 (Older) & 30 (Younger), Com |
NR (US) |
83.1 (80-91) & 25.5 (21-30) |
42.2% |
14 |
Diary |
ISD |
A |
A: Age |
None |
BTv & RTv: Younger > Older. |
|
Ogawa et al.
|
2011 |
Intervention |
1W BL, 2W placebo. |
380, Insomnia |
100% Japanese |
48.5 (17.0) |
63.2% |
7 |
Diary |
Categorical (BL SOL fluctuation <-30, +/-30,
>30min groups) & ISD |
A, D |
A: Age;
D: Insomnia. |
SOLm |
SOLv: ~ +age, +habitual SOLm, -habitual TSTm, past
benzodiazepines use; significantly greater SOL
reduction in those with larger BL SOL fluctuation
(<30 & >30 min) compared with smaller
(±30min). |
|
Okun et al.
|
2011 |
Observational |
1 or 2 wk baseline Diary. |
222 Com (older) |
94.1% White |
73.7 (7.1) |
67.1% |
7 or 14 |
Diary |
ISD |
B, D |
B: Inflammation biomarkers (IL-6, TNF-α);
D: Group (Good Sleepers, Insomnia, Bereaved,
Carers). |
Age, sex, BMI, SF-36, depressive symptoms,
stress |
- BTv: NS b/w groups; ~ +TNF-α;
- RTv: Good Sleepers < other groups; ~
+IL-6 in Good Sleepers.
- TIBv: Good Sleepers < Insomnia, ~ +IL-6
in Good Sleepers;
- TSTv: Good Sleepers < other groups.
|
|
Ong et al.
|
2007 |
Observational |
1W Diary at BL, comparing Morning, Intermediate, &
Evening chronotypes. |
312 Insomnia |
NR (US) |
48.86 (14.08) |
59.0% |
7 |
Diary |
ISD |
C |
C: Chronotype in insomnia patients |
TWT |
- BTv: NS group difference (univariate);
- RTv: Evening > Morning/Intermediate
chronotypes (univariate);
- Evening chronotype more variable BTv & RTv
(multivariate).
|
|
Patel et al.
|
2014 |
Observational |
1W Actigraphy. |
6038 Com (older) |
NR (US) |
79.91 |
49.4% |
≥5 for M, 3 for F |
Actigraphy (with Diary) |
ISD |
A, B, C |
A: Race;
B: health outcomes;
C: Cognitive function, antidepressant use. |
TSTm, demographics, mental/physical health history,
antidepressants, benzodiazepines, life style factors,
cognitive function. |
- SMv ~ +minority race, +diabetes, +heart
failure, +antidepressants, -cognitive function,
-subjective health, -TSTm, +BMI in M (not F),
+obesity in F (not M);
- TSTv ~ +minority race, +diabetes, +coronary
artery disease, +heart failure,
+antidepressants, -cognitive function,
-subjective health, -TSTm, +BMI, +obesity.
|
|
Roane et al.
|
2015 |
Observational |
Diary for 9W at the start of university. |
132 Uni |
62.9% White, 18.9% Hispanic |
18.6 (0.4) |
54.0% |
Average 56 |
Diary |
Mean range of a 4-day moving window |
A, B, C |
A: Sex, ethnicity;
B: Weight changes;
C: Depressive symptoms, chronotype. |
Sex, ethnicity, depressive symptoms, chronotype,
interaction b/w sex & sleep variables |
- BTv: ~ +weight gain, +eveningness, NS ~
sex, ethnicity, depressive symptoms;
- RTv: M >F, ~ +weight gain, +eveningness,
NS ~ ethnicity, depressive symptoms;
- TSTv: NS sex difference; significantly
predicted weight gain for F but not F.
|
|
Roumelioti et al.
|
2010 |
Observational |
Up to 2W Diary for pts, 1W for Ctrl. |
183 pts (CKD, ESRD) & Ctrl |
74.3% White |
52.65 |
37.2% |
14 & 7 |
Diary |
ISD |
B |
B: CKD & ESRD |
Age, sex, & race |
Qualityv: ESRD > CKD > Ctrl; NS ~ phosphorus
level, hemoglobin, bicarbonate & diabetes. |
|
Rowe et al.
|
2008 |
Observational |
1W home Actigraphy & Diary. |
133 Com (older carers of dementia & noncarers) |
96.2% White |
72.31 (7.04) |
66.3% |
7 |
Actigraphy & Diary |
CV |
A |
A: Care-giving of dementia patients |
Age, education, depression, total Nr of
medications |
- TSTv: Carers > non-carers both
Actigraphy & Diary;
- SEv: Carers > non-carers both Actigraphy
& Diary;
- SOLv: NS group difference on either
Actigraphy or Diary;
- WASOv: NS group difference on either
Actigraphy or Diary;
- Qualityv: NS group difference.
|
|
Sánchez-Ortuño & Edinger
|
2012 |
Intervention |
RCT on 4 biweekly CBT-I vs Sleep Hygiene for PI or
CMI, POST & 6 month FU assessments. |
81 Insomnia |
58% White |
54.2 (13.7) |
12.5% |
14 |
Actigraphy & Diary |
ISD |
D |
D: Type of insomnia, subjective sleep, treatment
related changes. |
None |
If not specified, findings apply to both subgroups
or both Actigraphy & Diary.
Total sample during BL:
- TSTv & SEv: CMI > PI (trend); PI (not
CMI) Actigraphy (not Diary) TSTv ~ +PSQI.
- SOLv: CMI > PI (Diary not Actigraphy);
NS ~ PSQI.
- WASOv: NS CMI vs PI; ~ +PSQI in PI (not
CMI).
Change based on CBT-I sample:
- TSTv, SEv, SOLv, WASOv: BL > POST on
Diary (not Actigraphy), NS POST vs FU;
- NS b/w BL TSTv, SEv & FU PSQI; BL
Actigraphy (not Diary) SOLv in PI (not CMI), &
BL Actigraphy (not Diary) WASOv in CMI (not PI)
~ +PSQI at FU.
- POST Diary SEv, SOLv, WASOv (but not TSTv)
reduction ~ +reduction in PSQI in CMI (not
PI).
|
|
Sánchez-Ortuño et al.
|
2011 |
Observational |
2W Diary in PI or IMD. |
187 Insomnia |
59.7% White, 33.9% Black |
47.14 (14.53) |
67.7% |
14 |
Diary |
MSSD |
D |
D: Subtype of insomnia |
Sex |
- TSTv: IMD > PI;
- SEv, SOLv, WASOv: NS b/w PI & IMD.
|
|
Shen et al.
|
2008 |
Experimental |
2W BL, 4W experimental phase for irregular
participants. Experimental group: increase regularity
of BT, RT, routines with review & weekly feedback; Ctrl
group: learn factors affecting performance. |
62 Uni (bipolar spectrum) |
71.8% White, 11.3% Black |
19.70 (18-24) |
71.8% |
14 |
Diary |
ISD |
C, E |
C: Mood lability, bipolar manic & depressive
symptoms |
None |
- TSTv: during BL, TSTv ~ +depressive
symptoms (small), higher across-day symptom
variability (small); NS ~ manic symptoms,
within-day symptom variability. During
Experimental phase, significant decrease for
both groups; decrease Experimental > Ctrl.
End of Experimental phase, Experimental (large)
but not Ctrl group significantly less variable
than BL.
- Increased lifestyle regularity did not
result in changes in correlates.
|
|
Signal et al.
|
2007 |
Observational |
1W Actigraphy & Diary at ~24W gestation (T1), 1W
before delivery (T2), 1W after delivery (T3), 6W/7W
postpartum (T4). |
19 Healthy (pregnant) |
NR (NZ) |
34 (29-40) |
100.0% |
7 |
Actigraphy(with Diary) |
ISD |
B |
B: Gestation, postpartum stage |
Parity |
All variables changed significantly over time, T3
most variable:
- TIBv: T2, T3 > T1, T4;
- TSTv: T3 > T1, T4;
- SEv, WASOv, IIV of 24hr sleep episodes: T3
> T1, T2, T4.
|
|
Suh et al.
|
2012 |
Intervention |
1W Diary at first & last week of a 7-session CBT-I
group program. |
455 Insomnia |
NR (US) |
48 (14) |
57.6% |
7 |
Diary |
Composites from MSSD of sleep variables |
A, C, D |
A: Age;
C: depressive symptoms, chronotype;
D: Insomnia, treatment response. |
Age |
Behavioural Schedule Component Score (BCS): BTv,
LOv, WTv, RTv, TIBv; Insomnia Symptom Composite
Score (ICS): SOLv, WASOv, TSTv.
- BCS: ~ -age (BTv, LOv, TIBv), +eveningness
(all 5 variables), +depressive symptoms (LOv,
WTv, RTv, TIBv), NS ~ ISI. Independent
predictors of BCS are +eveningness, +depressive
symptoms, & their interaction (BCS ~
+eveningness among those with higher but not
lower depressive symptoms).
- ICS: ~ +depressive symptoms (TSTv), NS ~
ISI or chronotype.
- CBT-I reduced IIV in all sleep variables
except BT & LO. High BL BCS group had
significantly higher BL & reduction in
depressive symptoms. ISI decreased, but NS b/w
high vs low BL BCS or high vs low BL ICS
groups.
|
|
Taub & Hawkins
|
1979 |
Observational |
2W sleep chart for regular vs irregular
groups. |
36 Uni |
NR (US) |
18-24 |
0.0% |
14 |
Sleep chart with 30min periods |
Categorical "regular vs irregular" based on
questionnaire, confirmed on CV |
C |
C: Personality traits |
None |
Irregular group lower on: dominance, sociability,
self-acceptance, self-control, achievement via
conformance, & intellectual efficiency, but higher on
flexibility. |
|
Vanderlind et al.
|
2014 |
Observational |
3W Actigraphy sandwiched b/w two assessment
sessions (T1 & T2). |
35 Uni |
NR (US) |
19.83 (1.25) |
40.0% |
21 |
Actigraphy (with Diary) |
ISD |
C |
C: Depressive symptoms, subjective sleep, genes,
cognitive control |
None |
TSTv: small correlation with T1 +depressive
symptoms, NS ~ T2 depressive symptoms; small
correlation ~ -cognitive control; NS ~ PSQI or
rs11932595 (gene). |
|
Waters et al.
|
2011 |
Observational |
4W home Actigraphy with Diary comparing
schizophrenia Pts & Ctrl. |
13 Schizophrenia Pts & Ctrl |
NR (AU) |
43.56 (6.48) |
30.8% |
28 |
Actigraphy (with Diary) |
ISD |
C |
C: Schizophrenia psychopathology |
None |
- TSTv: Pts > Ctrl (trend);
- SEv & SOLv: Pts > Ctrl (trend).
|
|
Westerberg et al.
|
2010 |
Observational |
2W home Actigraphy & Diary. |
20 aMCI, Ctrl |
NR (US) |
71.8 |
75.0% |
14 |
Actigraphy & Diary |
ISD |
C |
C: Cognitive function |
None |
TIBv, TSTv, SEv, & SOLv: NS b/w groups; ~ -logical
memory (small - moderate), but NS ~ 24-hr
recognition. |
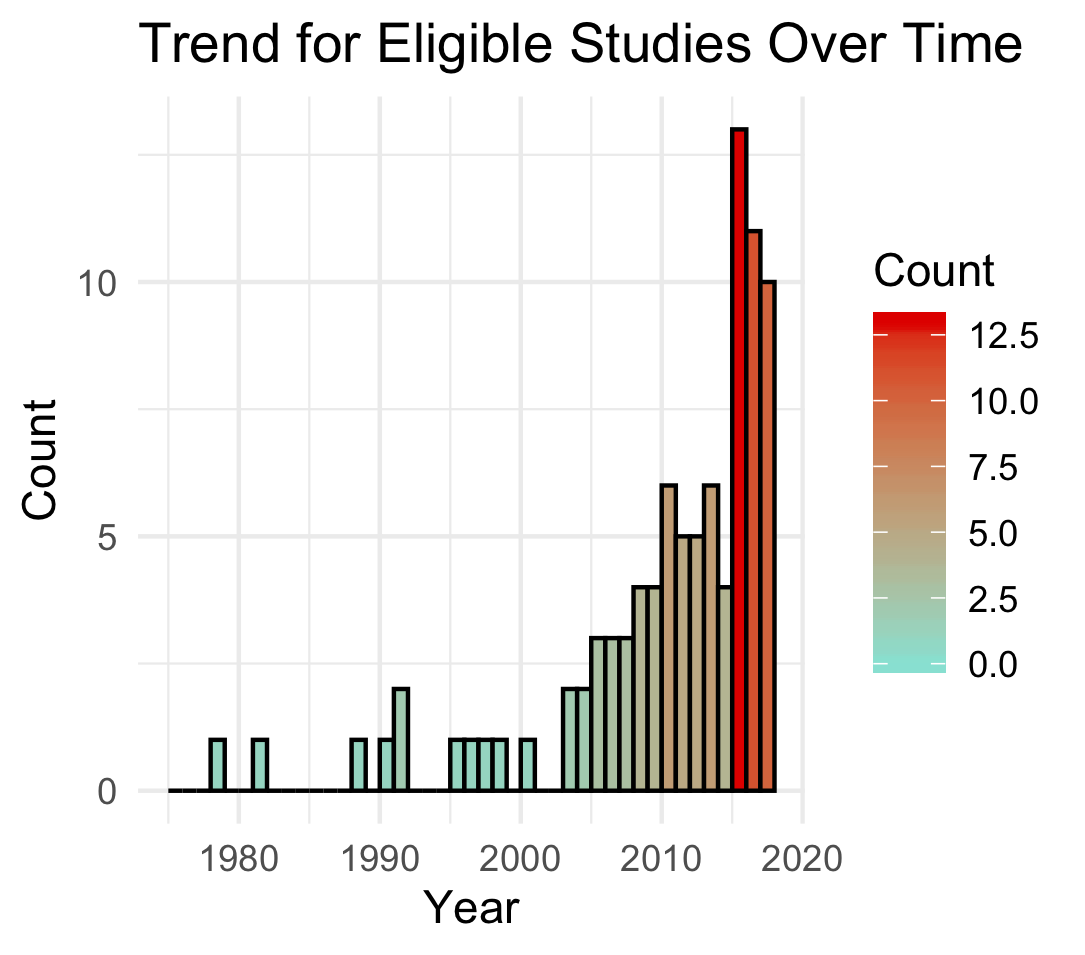 On this website, you will find an ongoing systematic review on
the correlates of sleep IIV, and information on methodologies in
researching IIV. We try to update this site regularly. A major
update using
On this website, you will find an ongoing systematic review on
the correlates of sleep IIV, and information on methodologies in
researching IIV. We try to update this site regularly. A major
update using